As co-blogger Mike wrote about on Wednesday, 10 month old Charlie Gard has lost his fight:
"The parents of terminally-ill baby Charlie Gard are 'utterly distraught' and facing fresh heartbreak after losing their final appeal in the European Court of Human Rights."
And, as Mike pointed out, there is true irony in the court's name.
But it's his conclusion that I think needs to be magnified:
"It would not be different in America."
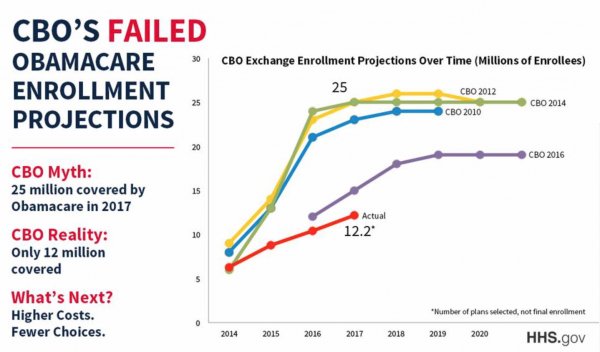
Here, Mike's referring to that ultimate progressive utopia: a government-run, single payer health care system. And this is the true moral of little Charlie's story: it's clearly not about the money, but has always been about control.
How do we know this?
Very simple: they explicitly told us.
Hunh?
Well, go back and read the Daily Mail story that Mike linked. Charlie's parents weren't asking for special care, or special funding, or that the Much Vaunted National Health System© (because ultimately, they own this) do anything more than get out of the way. They had already successfully raised almost $2 million in order to take him to the US for a promising therapy trial. It would have cost the MVNHS© (and the European Court) exactly nothing to let him go.
Well, that's not entirely true: because if they let Charlie go, well, Katie bar the door.
It's all about control. And if you like the idea of the IRS (for example) deciding who gets care - and who doesn't - well, be careful what you wish for.
"The parents of terminally-ill baby Charlie Gard are 'utterly distraught' and facing fresh heartbreak after losing their final appeal in the European Court of Human Rights."
And, as Mike pointed out, there is true irony in the court's name.
But it's his conclusion that I think needs to be magnified:
"It would not be different in America."
Here, Mike's referring to that ultimate progressive utopia: a government-run, single payer health care system. And this is the true moral of little Charlie's story: it's clearly not about the money, but has always been about control.
How do we know this?
Very simple: they explicitly told us.
Hunh?
Well, go back and read the Daily Mail story that Mike linked. Charlie's parents weren't asking for special care, or special funding, or that the Much Vaunted National Health System© (because ultimately, they own this) do anything more than get out of the way. They had already successfully raised almost $2 million in order to take him to the US for a promising therapy trial. It would have cost the MVNHS© (and the European Court) exactly nothing to let him go.
Well, that's not entirely true: because if they let Charlie go, well, Katie bar the door.
It's all about control. And if you like the idea of the IRS (for example) deciding who gets care - and who doesn't - well, be careful what you wish for.